The primary purpose of a nation’s healthcare system is to provide easy and high quality access to healthcare, and deliver it at an affordable price to its citizens. This is amid an onslaught of unceasing societal change. Population growth, the prevalence of chronic diseases, ageing and threats of epidemics—combined with the limitations of hospital infrastructure and number of doctors—imply that the time-honoured but costly method of delivering healthcare through face-to-face consultation and interaction between the patient and doctor can no longer match the huge demand.
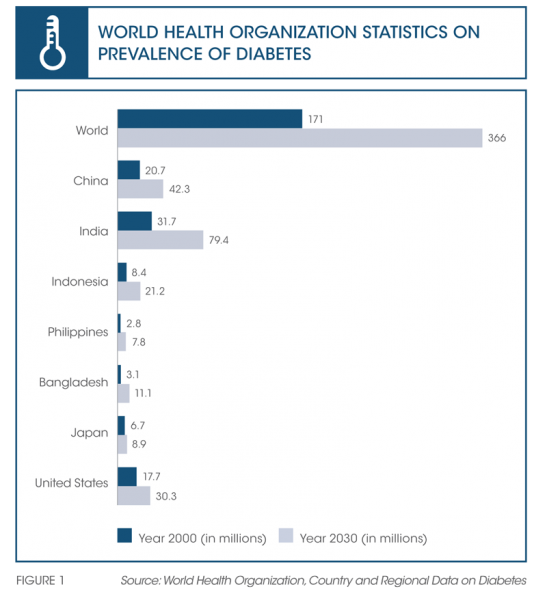
The incidence of chronic diseases—lifelong conditions that cannot be cured, such as diabetes, hypertension and asthma—is on the rise. This is a point of concern for governments and their public policy advisors, who warn that the financial burden of healthcare will require significant sacrifices through increased taxation or the peeling back of benefits to citizens. Today, up to 860 million people worldwide have one or more chronic conditions.1 In the case of diabetes alone, the World Health Organization (WHO) statistics show that the number of diabetics the world over will increase from 171 million in 2000 to 366 million in 2030 (refer to Figure 1).2
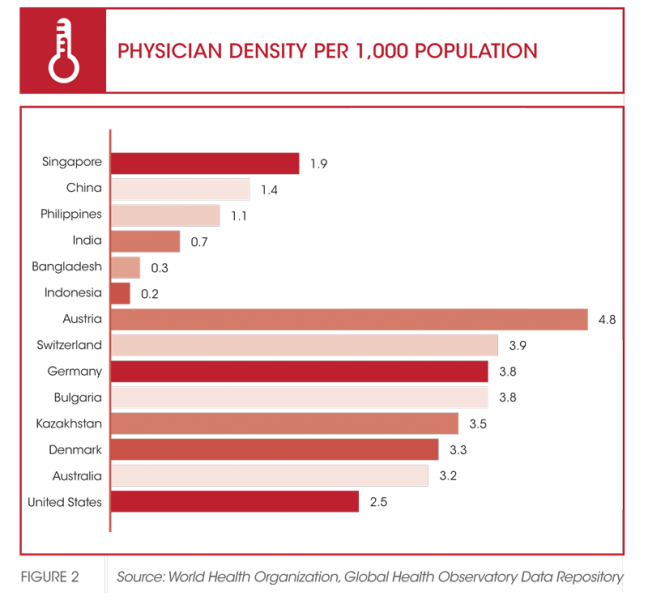
A particular challenge is how to bring healthcare to needy citizens, especially in remote or rural areas, where a patient may need to travel up to hundreds of kilometres to reach a tertiary medical centre. Physician density gravitates towards urban centres where healthcare infrastructure, including specialist facilities, is more developed. Doctors and healthcare providers prefer to practice in these centres as they provide enhanced income opportunities.
Meanwhile physician density in rural and provincial locations continues to be limited, partly due to undeveloped or underdeveloped infrastructure. And often, in the absence of medical staff and infrastructure, many patients in countries such as Malaysia, Indonesia, the Philippines and even India choose to rely on alternative remedies and medicines. While it is acknowledged that such medicines will always co-exist with and complement modern medicine, self-medication remains unregulated and dangerous, many a time leading to the worsening of an already chronic condition (refer to Figure 2).
The technology-enabled wellness revolution
Aided by advances in information and communications technology (ICT), the evolution of healthcare is continuing—it is a work in progress that has evolved from curative, to preventive, to pre-emptive (or wellness). So thorough has the progress been that there would be few people today who have not undertaken some form of wellness activity in the last 30 days—be it a fitness programme, a dose of vitamins or a pre-emptive test for hypertension or cardiovascular health. Many of these are sponsored workplace activities or part of an employee benefits package.
Aimed at keeping the human machine in prime condition, consumers are being seduced by wearable technology such as wristbands, health trackers and mobile phones that monitor wellness indicators. Over the last five years, thousands of apps have been developed to cover every life event from pregnancy (BabyBump PregnancyPro) to diabetes support (GlucoseBuddy). Many are free. A limited number of apps are also available for medical professionals, such as ones that provide reference material on drugs (MIMS) and other content, or help with administrative tasks (timekeeping).3
In some countries, physicians have access to government administered Electronic Medical Records (EMR) repositories, but this is a patient preference and approval is not automatically given to medical staff. Hospitals are generally better served than individual physicians when it comes to adopting information technology, with hospital information systems as well as EMR facilities meeting the need for continuity of care from hospital to home.
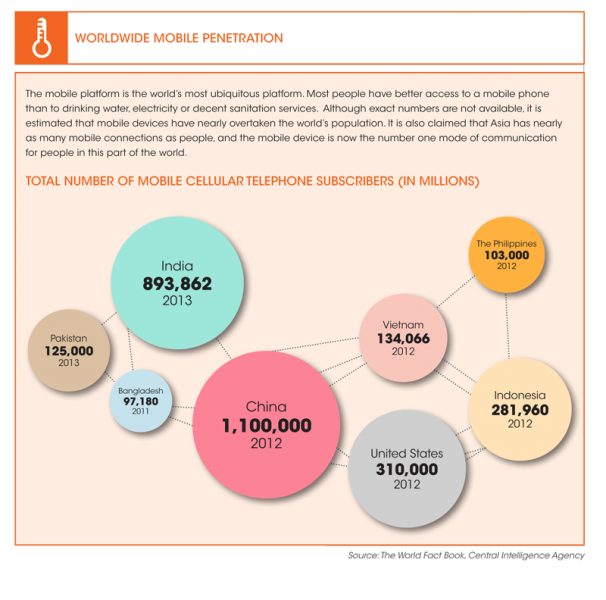
To address the rising incidence of chronic disease, the shortage of facilities and staff, and the need for extending care outside the hospital or clinic, a new healthcare ecosystem is emerging that leverages mobile technology. It is another step in the transformation of medical care and mirrors the changes in patient management that have taken place over the last few decades. While mobile technology is an obvious solution, the critical factor here is not only the technology solutions developed, but also their interoperability in relation to technology standards. Here, interoperability relates to the connections between the various elements of the integrated solutions—such as medical devices, applications and the seamless flow of medical information—and the healthcare system.
Evolution of a new mobile health (mHealth) ecosystem
Improvement in telecommunications and technology implies doctors are now able to receive details of a patient’s vital signs, medical images and laboratory results ahead of an initial assessment. At the core of the new approach to ‘telehealth’ is mobile technology, which provides a communications platform between patients and healthcare providers, and enables remote and isolated communities to access healthcare.
The distant communication between healthcare providers and patients is known as ‘telemedicine’, which comes from the Greek word ‘tele’ meaning ‘at or over a distance, far, complete and end of a task’. But telehealth is broader in scope than telemedicine. The myriad technology solutions and services offered under telehealth include teleconsulting via mobile phone between doctors; remote surgery; chronic disease management (CDM) and preventive care; specialised care support centres for hypertension, diabetes and dementia; patient education and support services; home monitoring and many more. Meanwhile, the use of mobile devices such as handsets, tablets and similar devices employed in the practice of medicine and public health is referred to as mHealth or mobile health. The devices are used to receive, send and monitor personal and clinical health data via cellular transmission to healthcare providers in real time, in order to enable an immediate response to a patient. Following the growing sophistication of cellular or mobile connectivity, telehealth and mHealth are now converging.
There is nothing new about telehealth; and its emergence probably dates back to the passing of the house call era. The next stage was one of simple phone calls—physician or patient initiated—that enabled monitoring of healthcare delivery and follow-up at home. However, drawbacks to this system included the fact that most calls were informal consultations and lacked quantifiable information. While physicians were probably happy to accept calls from the patients they were close to, problems arose when the volume of calls escalated and began eating into their face-to-face practice and personal time.
Nowadays, many modern clinics offer a concierge service. Operated by private companies, these call desks screen and/ or address questions from patients. Hospitals, too, have a similar service with hotlines available and connected to the Accident and Emergency (A&E) unit. But both systems are at a loss when it comes to providing care for patients who are unable to come to a hospital or other health facilities. In days gone by, lengthy stays in hospital would have been followed by house calls, visits from the district nurse, or private nursing services (which are still available at a cost to the patient or the government).

Since the turn of this century, telehealth systems supported by mobile devices have been increasingly used to address chronic disease monitoring, health education, and treatment and support services. Use of telehealth solutions can also provide data collection and remote monitoring services, disease surveillance and drug adherence, health information systems, point-of-care, and emergency medical services. As such, they easily fulfil the primary aims of an efficient health service—to improve access, affordability and quality.
In Singapore, telehealth solutions for patients suffering from chronic diseases, such as hypertension and diabetes, have helped government hospitals manage their patient flow more efficiently. Examples of such companies include TeleMetrix+, a commercial cloud-based telehealth service that enables doctors to remotely monitor and track patient vital signs in the comfort of the patient’s home; Connected Health, a remote health monitoring solution that allows healthcare, nursing, and fitness service providers to improve care, reduce costs and increase productivity; and REKA Health which develops and markets innovative telehealth solutions through an interactive health technology platform consisting of electrocardiogram (ECG) medical devices, application software, mobile apps, cloud-based web applications and Personal Health Records (PHR).
Similarly, in Japan there are more than 20 such solutions, including primary care clinics that cater to self-monitoring individuals. Both Malaysia and the Philippines, too, have active telehealth associations.
The development of telehealth and remote monitoring systems over the last ten years has enabled medical staff to reduce congestion at the hospital and other health facilities by extending medical facilities and enabling recovery at home. A major benefit of efficient telehealth solutions is the seamless transmission of medical data from the patient to the hospital, which allows patients and healthcare providers to access feedback and communicate whenever and from wherever they desire.
Since the turn of this century, telehealth systems, supported by mobile devices, have been increasingly used to address chronic disease monitoring, health education, treatment, and support services.
Interoperability
Interoperability involves the design of standardised guidelines for wireless medical devices at home, and a mode of transmission in a format that is compatible with the health information exchange standards followed by connected health devices and systems. These include tablets, smartphones, gateways and remote monitoring devices. The standards provide a framework for delivering clinical quality medical information from a remote consumer environment to the hospital through the devices.
For example, in the hospital environment, information about the patient is kept in the hospital EMR. However it is equally important to have vitals signs measured and followed up on after the hospital stay, in order to have full documentation of the patient’s recovery. But vital signs taken at home can only be recorded if they are in a format compatible with the relevant EMR and health information system.
For patients, standardisation will enable easy connectivity with personal connected health tools to allow consumers to create individual, interoperable, customised networks of devices and services to manage their health.
While telehealth can function in the absence of interoperability, interoperability in technology and solutions design standards fuels telehealth adoption and is a key factor in ensuring access and affordability. When functioning effectively, it can dramatically improve health management, clinical outcomes and quality of life by empowering information-driven health self-management.
While telehealth can take place in the absence of interoperability, interoperability fuels telehealth adoption.
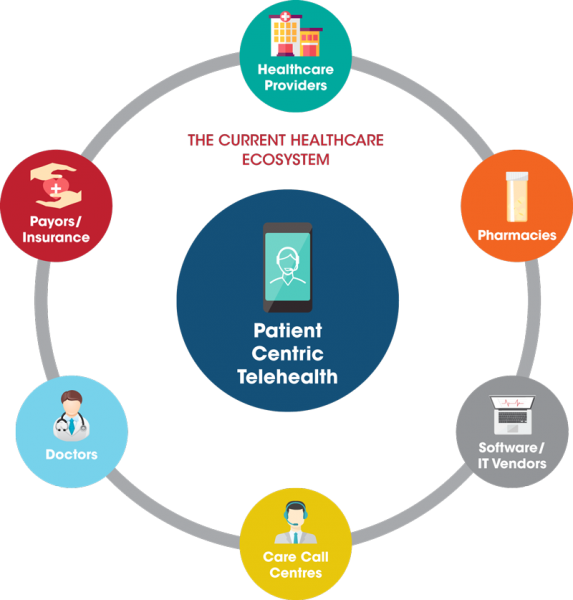
The current healthcare ecosystem
An integrated, interoperable telehealth solution would go a long way towards offering the three factors that are key for any successful health programme: access, affordability and quality. However, it is also a fact that technology-dependent telehealth solutions are more likely to be found in countries where the government subsidises healthcare, such as Japan and Singapore.
One of the greatest challenges to increasing the adoption of telehealth services is the need for better and closer collaboration among all partners and stakeholders in the telehealth ecosystem, including the government, insurance companies, regulatory bodies, hospitals, technology companies and medical device companies.
A more nuanced issue here is the proliferation of proprietary apps and systems, which represent factors that hinder scalability. Why? Because ‘closed’ or proprietary systems are generally costly, even though telehealth solutions have helped extend care to outside the hospital. Too many different companies delivering similar solutions will tend to result in more expense as their applications solutions are not technology standardised and therefore access is limited. Moreover, not only will the access goal be unmet, but a lot of data is likely to get lost or not used in the process. On the technology side, mobile device manufacturers and mobile service providers will need to work together as currently, there are far too many devices and solutions working independently.
Given the uneven physician-to-population density and increasing mobile access, there is no doubt that in the near future, there will be tremendous growth in telehealth as a means of delivering healthcare. A concerted effort to achieve common goals among the ecosystem’s stakeholders will see telehealth become mainstream practice.